
The FRONTIER Research Group is the largest specialist fronto-temporal dementia (FTD) clinic in Australia. Since 2007, we have specialised in the diagnosis, prognosis, and care of people with FTD
and related conditions. We also specialise in researching social cognition, neuroimaging, speech and language, behaviour, clinical management, and many other aspects related
to FTD and dementia more generally. We work with patients with FTD, Alzheimer's disease, and related diseases, including corticobasal syndrome (CBS) and progressive supranuclear palsy (PSP).
We collaborate with carers and families to help inform diagnosis and obtain important information about participants' functioning and cognitive change. Importantly, we aim to assist carers
through all stages of the FTD journey through education, psychosocial support, and referral to specialist services.
FRONTIER is headed by Professor Olivier Piguet and involves approximately 20 researchers, clinicians, neurologists, and administrative staff. Our work is supported by the government through the National Health and Medical Research Council, university funding, and community donations. Our clinic is located at the Brain and Mind Centre in the University of Sydney and is integrated with the ForeFront collaborative research network.
What is FTD?
FTD is a complex group of related diseases, including behavioural-variant FTD, semantic dementia and progressive non-fluent aphasia.
Who are we?
Come and meet the team of researchers, doctors, psychologists and professional staff who make up FRONTIER.
Participate
Are you interested in participating in our research, as a patient or a healthy control? Find out how to get involved below.
Frontotemporal dementia refers to a group of disorders caused by progressive degeneration of the frontal and/or temporal lobes of the brain. The majority of FTD cases occur between the age of 45 to 64 and affects both men and women.
The initial symptoms of FTD depend on which part of the brain is first affected.
- The frontal lobes are involved in planning, attention, decision-making, mood and empathy. Damage to this region results in changes to personality and behaviour. This is known as behavioural-variant FTD (bvFTD).
- The temporal lobes are involved in understanding and expressing language. Damage to this region causes the decline of language skills. This is known as primary progressive aphasia (PPA), of which there are three variants: semantic dementia, progressive nonfluent aphasia, and logopenic aphasia.
The rate of decline varies, and can range from 2 to 20 years. As the disease progresses, more symptoms in behaviour, language or movement may appear as more regions of the brain are affected. Unfortunately, there is currently no cure for FTD, nor treatments to slow or stop disease progression. However, there are strategies to manage FTD symptoms that can help to maintain and improve quality of life for the person affected and their loved ones.
For more information about the subtypes of FTD, click here.
If you or a loved one has recently been diagnosed with FTD and would like some advice, click here.
A glossary of common terms surrounding FTD is listed here.

Prof. Olivier Piguet
Director, FRONTIER Professor of Neuropsychology
Associate Prof. Rebekah Ahmed
Neurologist Clinical Associate Professor
Associate Prof. James Burrell
Neurologist
Dr. Emma Devenney
Neurologist
Dr. Yun Hwang
Neurologist
Prof. Kirrie Ballard
Professor & Speech PathologistProf. Muireann Irish
Professor of Cognitive Neuroscience
Associate Prof. Fiona Kumfor
Senior Research Fellow Clinical Neuropsychologist
Dr. Ramon Landin-Romero
Seneior Research Fellow & Senior Lecturer
Dr. Cristian Leyton
Senior LecturerPatients
If you have been diagnosed with frontotemporal dementia you have an important role to play in our research. Here’s what you need to get involved:
- A diagnosis of behavioural-variant FTD, semantic dementia, progressive non-fluent aphasia, logopenic progressive aphasia, corticobasal syndrome, progressive supranuclear palsy, or Alzheimer’s disease.
- Fluency in English
- Living at home
- Able to communicate and manage basic self-care
- Able to walk unaided
- No other major neurological or psychological disorders, such as major stroke, severe brain injury, schizophrenia or bipolar disorder.
We strongly recommend that you have a close family member or friend available to accompany you to the clinic, so that we can gather data from multiple perspectives.
If you, or someone you care for, meet these criteria and would like to participate in our research, ask your specialist (neurologist, geriatrician, or psychiatrist) to send us a referral at frontier@sydney.edu.au.
If you are driving or flying from outside of Sydney, FRONTIER will contribute to your travel expenses up to a maximum of $500 (e.g. petrol, flights, accommodation) so please keep your receipts.
If you require local accommodation, we can provide you with a list of recommendations that are all within walking distance from the clinic.
What research participation looks like
Research participation typically involves a two-day visit to the FRONTIER research clinic. You will:
- Have a session with one of our specialist neurologists.
- Complete questionnaires about your medical history and family history.
- Complete tests of your memory, language, and other thinking skills.
- Have an MRI scan of your brain – this is a painless, non-invasive procedure that generates high quality images of your brain.
- Be invited to give a sample of blood as part of our biomarkers research project (optional).
Healthy Volunteers
We are always in need of healthy volunteers to aid us in our research. Participating with us as a volunteer typically involves the activities mentioned above. If you would like to volunteer, please email frontier@sydney.edu.au.
Refer
Are you a neurologist or medical professional who would like to refer a patient to us for an expert opinion? Find out how below.
Carer Resources
Do you provide support to someone with dementia? Find out more about dementia management, services and support below.
Social Media
We actively post helpful information on our social media accounts. Find out more about how to engage with us below.
When to refer to us
If you are a GP or specialist and have a patient with a suspected diagnosis of one of the following diseases, please refer to FRONTIER for an expert opinion:
- Frontotemporal dementia (FTD)
- Behavioural variant FTD (bvFTD)
- Semantic dementia (SD)
- Progressive non-fluent aphasia (PNFA)
- Logopenic aphasia (LPA)
- Corticobasal syndrome (CBS)
- Progressive supranuclear palsy, or
- Alzheimer’s Disease
What to include
Please send all referrals via email to frontier@sydney.edu.au or via fax: (02) 8322 4000. When referring, remember to include:
- a description of the person, including the reasons for suspecting one of these diseases.
- copies of any neuropsychological tests the person has completed (e.g. MMSE, MoCA, ACE-III).
- copies of any imaging conducted (MRI, PET), including the radiologist reports.
Head to the dedicated carer section of this website for detailed information designed for carers and family members of individuals diagnosed with FTD, including:
- a list of general recommendations for a new diagnosis of FTD
- advice on responding to challenging behaviours
- help accessing the NDIS or MyAgedCare
- Further resources on support, education and services available to you.
Mobile Apps
We are currently adapting several neuropsychological tests from paper to tablet form. Find out more below.
Clinical Tests
We have developed a range of tests to help clinicians accurately assess cognitive function and diagnose frontotemporal dementia.
Our research
To date, FRONTIER has published over 550 peer-reviewed scientific articles on FTD. Find out more about the research we produce below.
The Sydney Language Battery

The Sydney Language Battery (SYDBAT) mobile app was developed to assist clinicians with the diagnosis of primary progressive aphasia and other language disorders.
Available now on the iPad app store and coming soon to Android.
ACEmobile
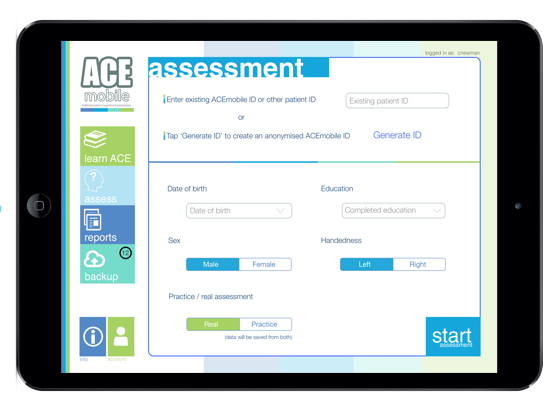
The ACEmobile is an electronic form of the popular Addenbrooke's Cognitive Examination III for Australian and UK versions.
Available now on the iPad app store!
FRONTIER has developed a range of neuropsychological tests and questionnaires to help clinicians accurately assess
cognitive function and behavioural changes and aid in the diagnosis of frontotemporal dementia. These tests, as well as other tests we have developed, are freely available to clinicians here.
Please note that these tests are not designed to be self-administered. Each test requires interpretation by a trained clinician in order to provide meaningful results.
Addenbrooke’s Cognitive Examination-III (ACE-III)
The Addenbrooke’s Cognitive Examination is a neuropsychological test used to identify cognitive impairment in dementia. The current version of the test is the ACE-III.
The ACE-III encompasses tests of five cognitive domains: attention, memory, fluency, language, and visuospatial processing. Scores are summed to give a total out of 100, where a score of 88 and above is considered normal cognition, below 83 abnormal, and between 83 to 87 inconclusive.
The Mini-Addenbrooke’s Cognitive Examination (M-ACE) is a shorter version of the ACE-III which is scored out of 30. Cut-off scores of 25/30 and 21/30 are recommended as diagnostic of a dementia syndrome.
The ACE-III protocols are available for download in English for hearing impaired adults, in English for remote administration, and in several different languages.
Sydney Language Battery (SYDBAT)
The Sydney Language Battery is a computer-based language test designed to identify patterns of deficits in expressive and receptive language abilities at the single-word level. It was developed to aid in differentiating between forms of primary progressive aphasia.
The SYDBAT consists of four subtests: Naming, Repetition, Comprehension and Semantic Association. Each subtest contains the same set of 30 nouns and is scored out of 30.
SYDBAT materials, administration and scoring guidelines, and cut-off scores for each subtest are available for download.
Cambridge Behavioural Inventory-Revised (CBI-R)
The Cambridge Behavioural Inventory is an informant-based questionnaire that evaluates the emergence of behavioural symptoms in dementia and other neurodegenerative brain disorders. The current version of the questionnaire is the CBI-R.
The CBI-R consists of 45 items evaluating 10 functional/behavioural domains: memory and orientation, everyday skills, self-care, abnormal behaviour, mood, beliefs, eating habits, sleep, stereotypic and motor behaviours, and motivation.
The CBI-R is completed by a family member or close friend. The frequency of a behaviour over the past month is rated on a scale of 1-4, where a higher score indicates greater frequency.
The CBI-R is available for download here.
Frontotemporal Dementia Rating Scale (FRS)
The Frontotemporal Dementia Rating Scale is an informant-based questionnaire that assesses the severity and rate of progression of frontotemporal dementia based on behavioural changes and functional dependence.
The FRS consists of 30 items evaluating 7 functional/behavioural domains: behaviour, outing and shopping, household chores and telephone, finances, medications, meal preparation and eating, and self-care and mobility. Scores on the FRS are categorised into six stages of disease severity, ranging from ‘very mild’ to ‘profound’ impairment.
The FRS is available for download here.
FRONTIER produces significant research output. Below is a summary of our most recent research papers (updated periodically). For the most up-to-date list of publications, please search for the profiles of any of our researchers individually.
| Title | Authors | Journal | Link |
|---|
Facebook
Follow our Facebook page for the latest updates in dementia care and research.
Twitter
Follow our Twitter page for what's happening in the research community.
Tweets by Frontier_UsydYoutube
Follow our YouTube page for videos about FTD, our research and lectures from our Carer Day.